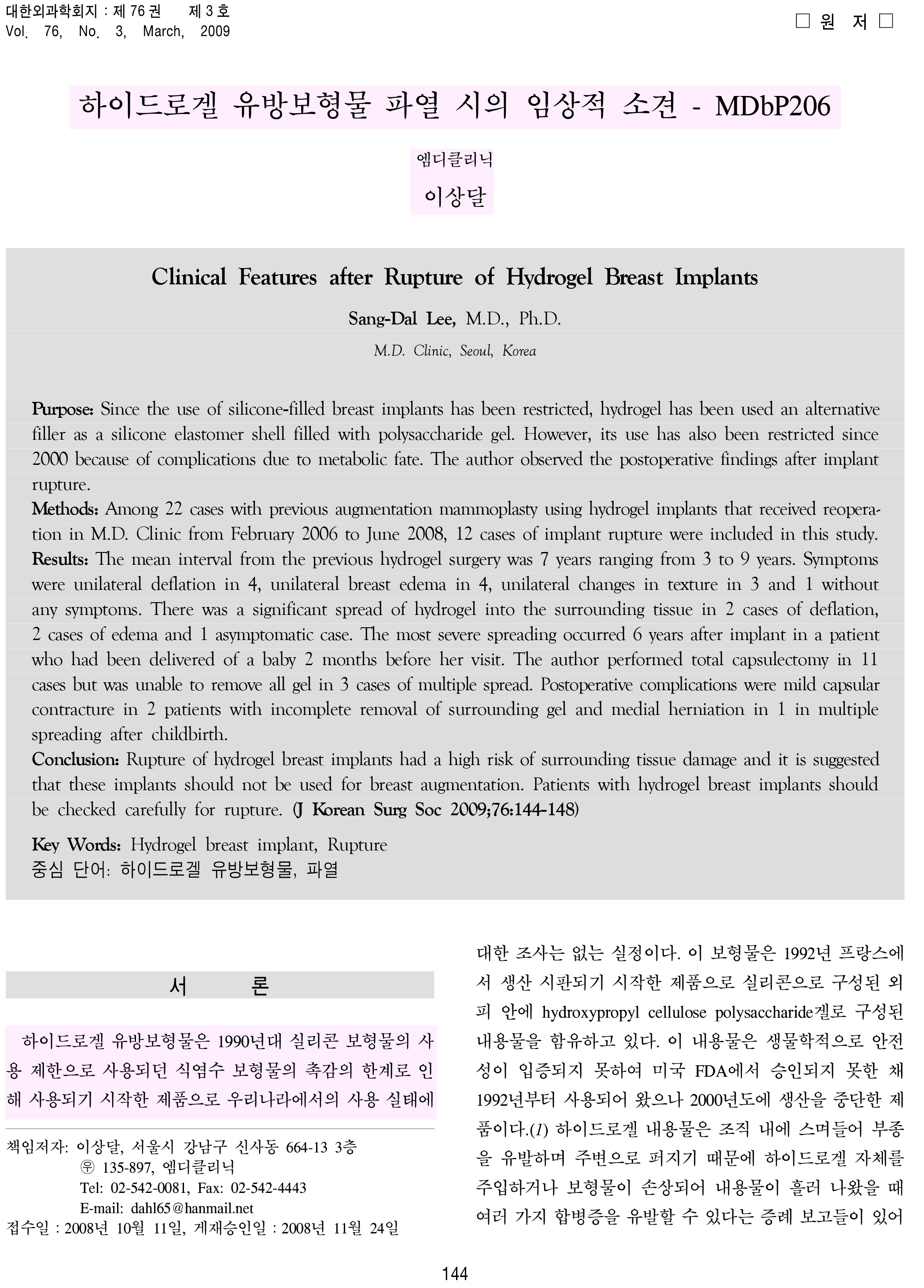
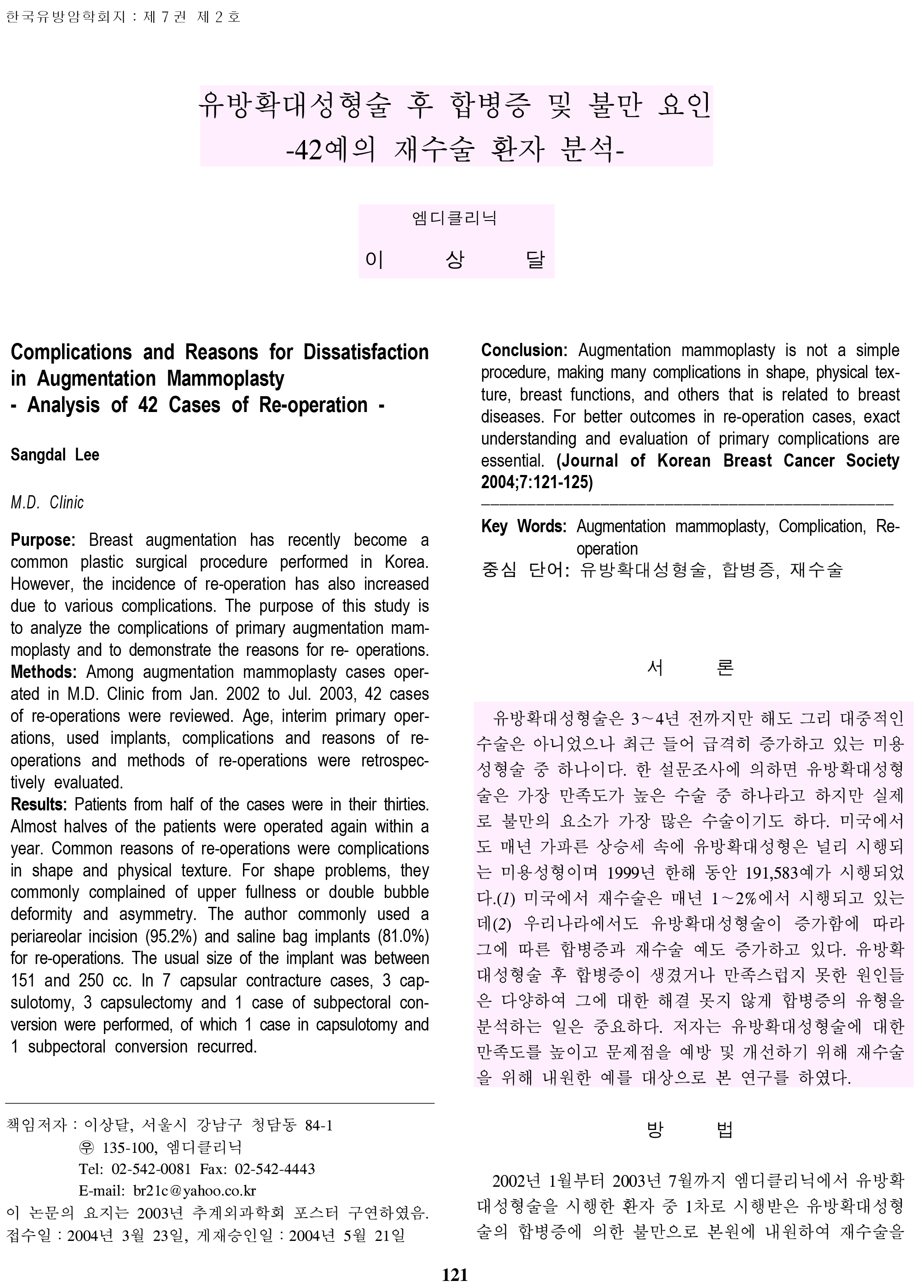
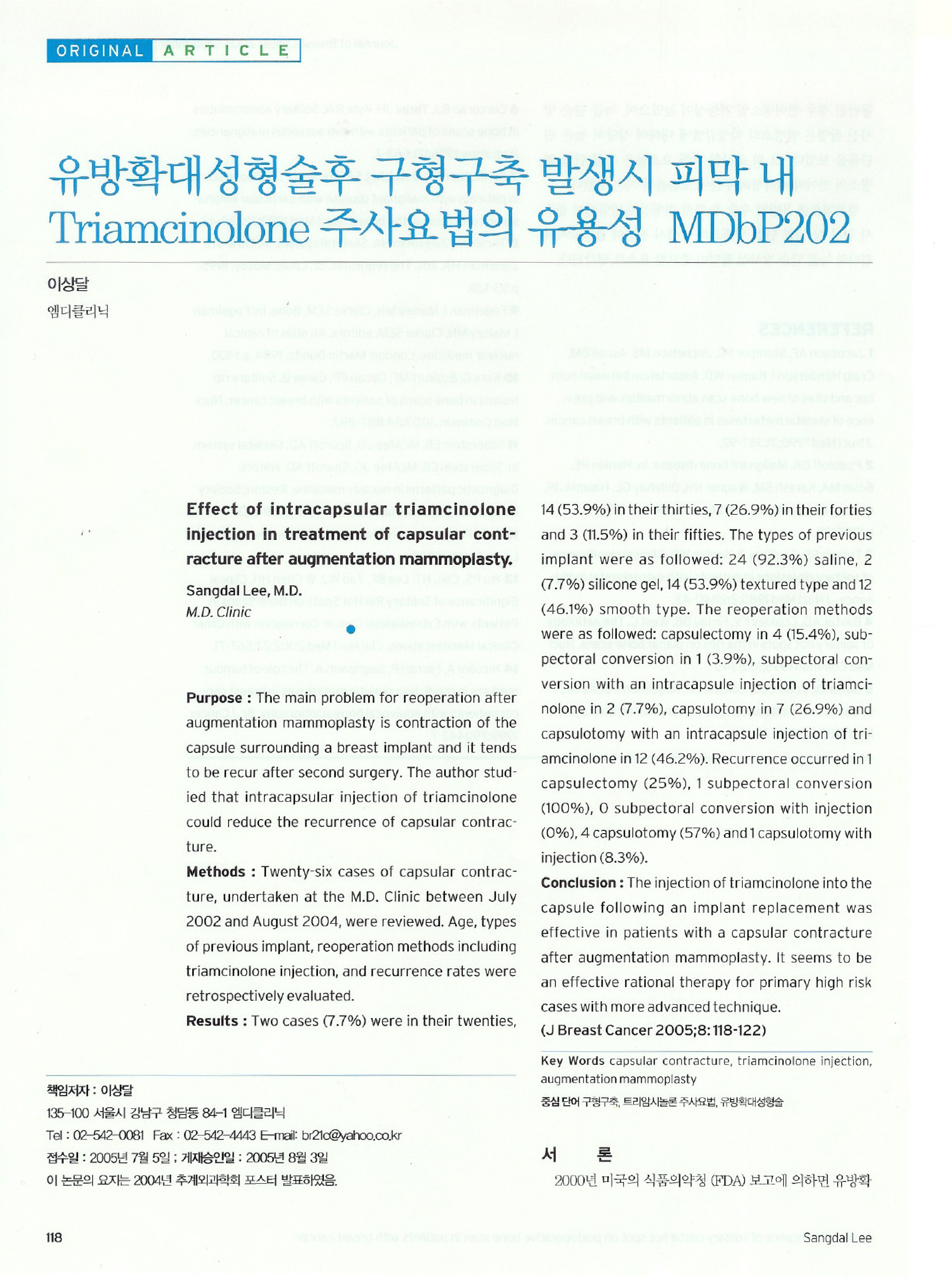
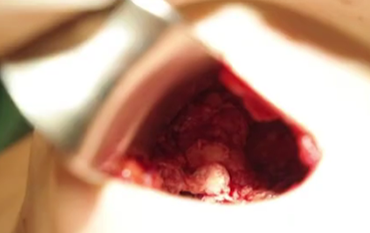
Remove the implant(capsular)
after incision of the inframammary
fold or armpit approximately 3.5 cm
-

Online consultation
-

WeChat consultation
-

Surgery review
-

Before-After
-

Location
TOP
TOP
breast revision surgery
Offering beautiful and healthy breast.
-
 Duration of surgery
Duration of surgery
1~2 hours
-
 Anesthetic method
Anesthetic method
General anesthesia
-
 Whether hospitalization is needed
Whether hospitalization is needed
1 day (Can be discharged on the same day)
-
 Removal of thread
Removal of thread
1 week later
-
 Treatment as outpatient
Treatment as outpatient
3~4 times (Forever AS)
-
 Recovery time
Recovery time
Within 1 week

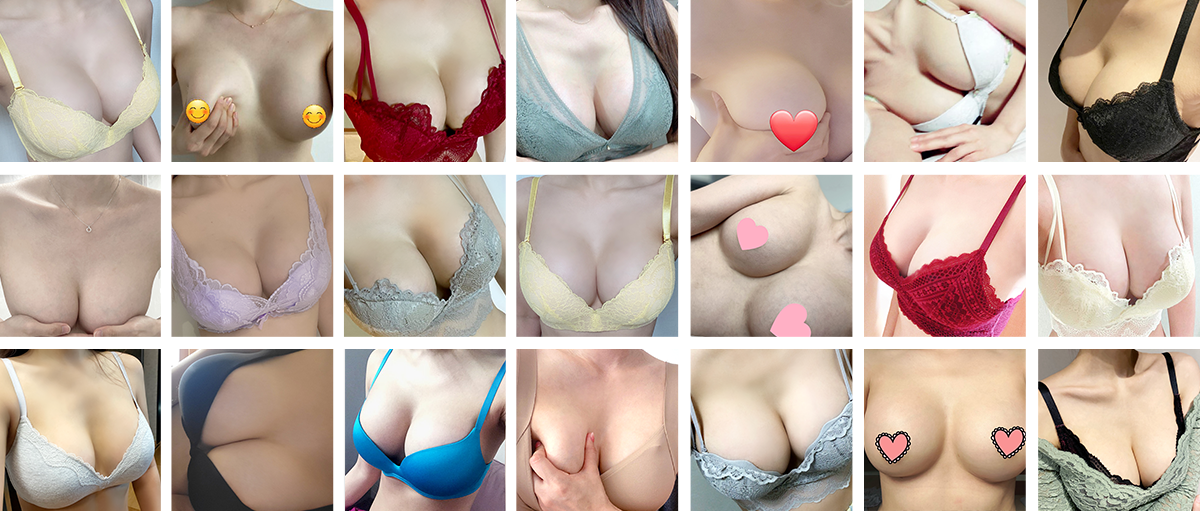
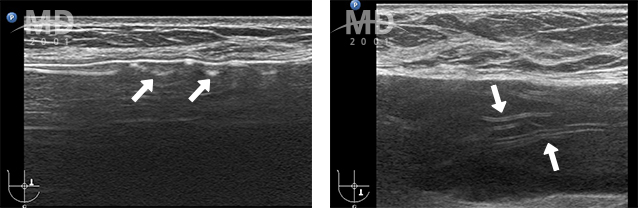
and soft tactile senses is the status of capsular!
“capsular,” which is a thin protective membrane that wraps around the breast to protect our body.
If this capsular gets deformed or thickens, abnormality in shape and tactile senses can occur.
-
Normal breast after the surgery
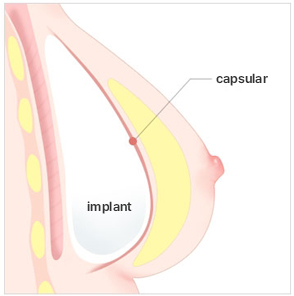 Thin and uniformly formed capsular to
Thin and uniformly formed capsular to
fit the implant -
Capsular formed thinly and uniformly in accordance with the implant
 Capsular formed abnormally too thick Capsular that became very thick and undulated
Capsular formed abnormally too thick Capsular that became very thick and undulated
formed too thin It is possible to realize natural looking waterdrop line
and soft tactile senses.
-
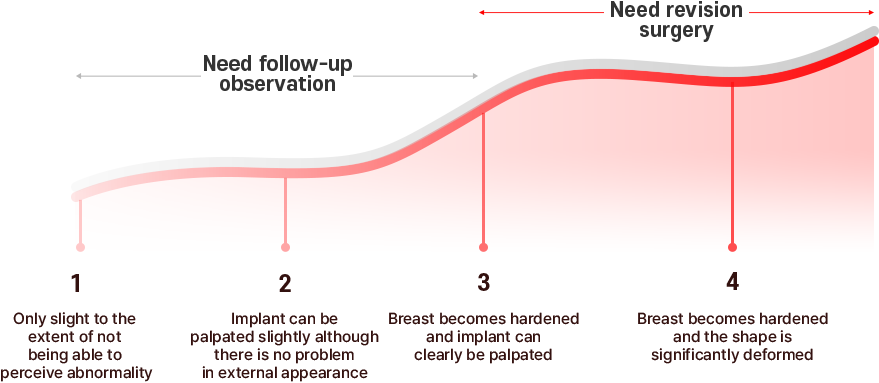
Implant status
(rupture/deformation) -
Capsular status
(thickness/position) - Whether the capsular is removed
- Side effect status
- Diagnosis of breast cancer and benign diseases
-

Blood test
-

Cardiography test
-

Chest x-ray
-

Breast scan
-

Ultrasound test
precisely diagnoses the conditions of the breast through a total of 5 examinations prior to breast revision surgery and conducts revision surgery through the method appropriate for the outcomes of the examinations performed. ※ Types of examinations can differ depending on the conditions of the patients.

-
Q1.
When is the appropriate time for breast revision surgery?
It is advisable to undergo revision surgery 6 months ~ 1 year after the initial surgery.
If you undergo revision surgery before the breast shape and tissues are properly established and settled down, unexpected side effects can be induced.
However, in the event of occurrence of rupture of implant or manifestation of capsular contracture, etc. for which treatment cannot be delayed, you need to undergo revision surgery as quickly as possible through consultation with the physician in charge. -
Q2.
Is revision surgery more painful than the initial surgery?
It is necessary to press the breast pocket for insertion of implant at the time of breast augmentation surgery, which induces pain.
However, since the tissues have been expanded in the initial surgery, pain actually tends to be less at the time of revision surgery. -
Q3.
Is the recovery period of revision surgery than that of the initial surgery?
There is marked difference among individuals.
The recovery period is 3~4 days at the minimum and 1~2 weeks at the maximum, making it similar to or slightly longer than that of the initial surgery.
ON BREAST REVISION SURGERY
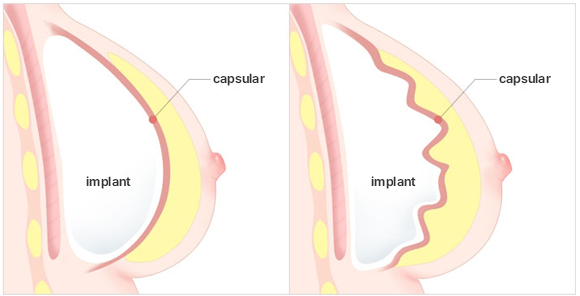
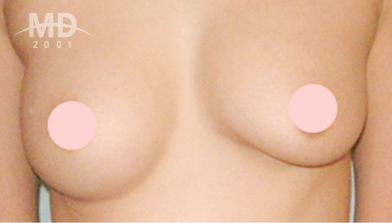
Capsular contracture

-
Definition
-
When implant is inserted into the breast, the body recognizes it as a foreign matter and forms capsular around it.
It is the side effect of excessive formation of this capsular and becoming hardened.
-
When implant is inserted into the breast, the body recognizes it as a foreign matter and forms capsular around it.
-
Cause
- Inflammation, hematoma due to hemorrhage, contamination due to foreign matter, neglectful of massaging after the surgery (smooth type) and physical constitution, etc.
-
Symptoms
- Breast becomes hardened and shape gets deformed
- Lose sensation or pain is induced
-
MD's Solution
- After having completely removed the hardened capsular that wrapped around the existing implant as well as the implant itself, replace with new implant to improve the shape and tactile senses.
-
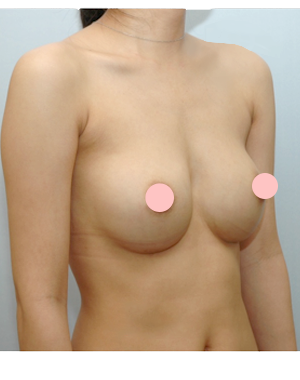
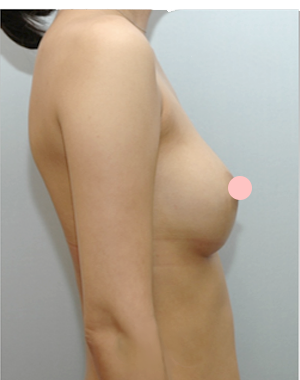
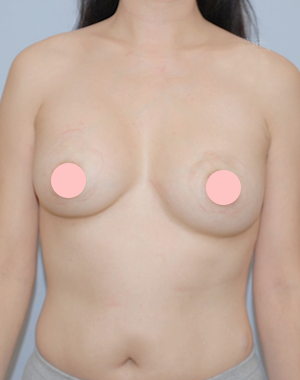
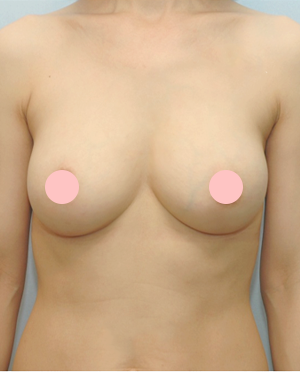
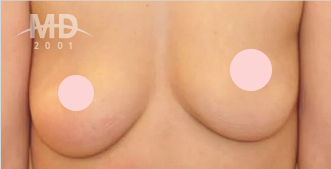
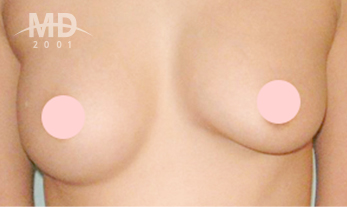
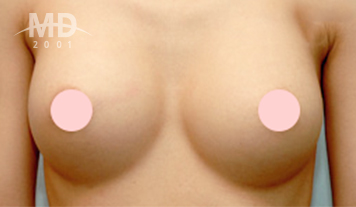
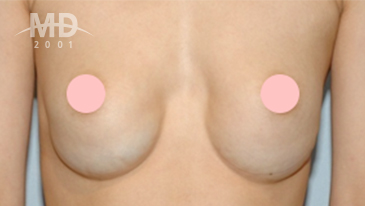
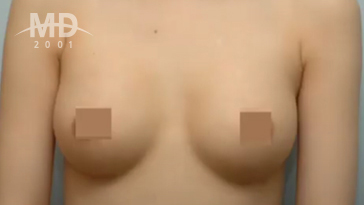
Before

-
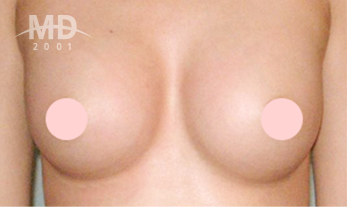
After

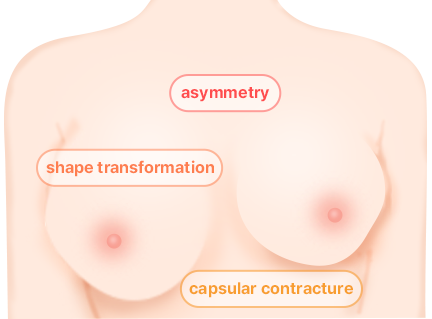
Capsular contracture step
MD's Capsular contracture prevention special solution
-
01
Special treatment during surgery
-
02
Operating room, which is a completely sterilized zone
-
03
Latest university hospital level medical devices
-
04
Systematic postoperative care
-
05
Rules that patients must abide by
Special treatment during surgery
-

Prevention of inflammation for Prevention of Capsular Contracture
Clean implant space with special antibiotic -
Administer suppressant for formation of fibroblast, which is the fundamental cause of formation of capsular
-
Prevent narrowing of breast pocket through treatment with adhesion inhibitor
-

Prevent capsular contracture through special treatment with capsular softener
Operating room, which is a completely sterilized zone
-

MD clinic is equipped with independent surgery center that has been designed as a completely sterilized zone, thereby significantly lowering the risk of infection.
-

Surgery in the morning and discharge in the afternoon the next day is the principle.
It is the principle not only for the safety of the patient but also to disinfect the entire operating room by turning on ultraviolet light in the afternoon. -

Access by unauthorized persons and items is prohibited by installing double door with fingerprint door lock and all the items brought in are subjected to thorough disinfection before they are taken in.
-

Vent system used only in some of the large hospitals is installed in the building to purify air in the operating room by sucking in and filtering out fine dusts.
-

Powder Free Glove, which is 2 times more expensive than ordinary surgical gloves, is used at the time of surgery to prevent entry of fine foreign matters into the operating room..
Latest university hospital level medical devices
-

Unnecessary exfoliation is prevented
and Bleeding is minimized by using the
latest freestyle endoscope -

Hemostasis is performed following precision surgery with
Ligasure hemorrhage prevention equipment to prevent capsular
contracture that can occur due to erroneous exfoliation
Systematic postoperative care
- step 01
- step 02
- step 03
- step 04
- step 05

- Penetrate special drug cocktail to the capsular area for 1 month after the surgery to assist formation of normal capsular.
- In the case of smooth implant, education on massaging is provided along with management of machine at the specialized management room and regular checkup.
- Take medicine for prevention of capsular contracture for 3 months immediately after the surgery.
- Prevent capsular contracture in advance through regular checkup by the attending surgeon on the 1st, 3rd, 6th and 12th months after the surgery.
- If capsular contracture occurs in spite of aforementioned measures, revision surgery is conducted.




Rules that patients must abide by
-

Make sure to take shower on the day of surgery! It is possible to minimize infection after the surgery only if you keep your body thoroughly clean since foreign matter can enter the body at the time of surgery if your body is not in clean state.
-

Taking capsular contracture prevention medicine! Since even the healthy patients can be infected by normal bacterial at the time of surgery, it is necessary to take capsular contracture prevention medicine to prevent activation of such bacteria in advance.
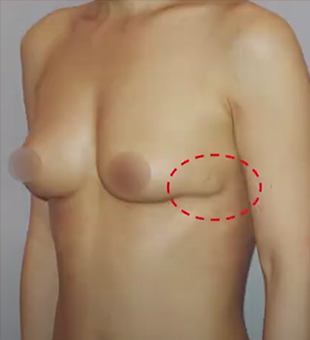
Upper pole fullness

-
Cause
- If exfoliation at the inframammary fold is insufficient
- If capsular contracture has formed
- If implant got lifted and fixated due to negligence in management after the surgery
-
Symptoms
- It looks unnatural with the upper portion of the breast protruding out in the shape of a rice bowl being put on upside down
-
MD's Solution
- Widen the breast pocket in comparison to the existing pocket to secure more space before inserting the implant.
- After having removed the hardened capsular that wrapped around the existing implant and the implant itself, replace with new implant to improve the shape and tactile senses.
-
Massage is essential for smooth implant while textured implant does not need massaging.
This must be adhered to thoroughly after the revision surgery.
In addition, brassiere with wire should not be worn for prescribed period of time after the surgery since it could cause the phenomenon of protruding upper portion with implant being pushed upward by such brassiere.
-
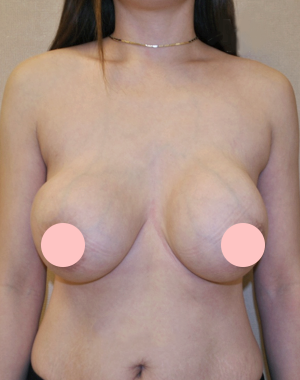
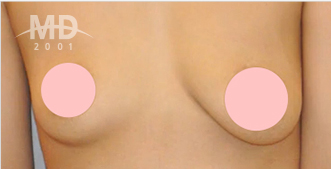
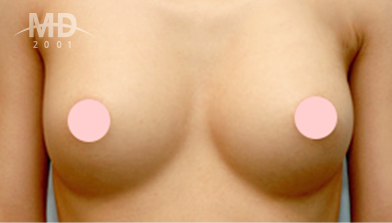
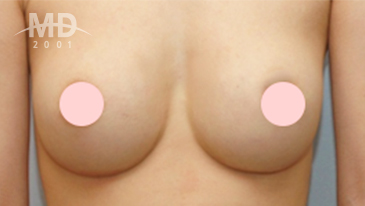
Before

-
After

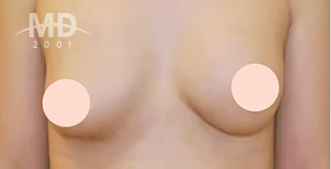
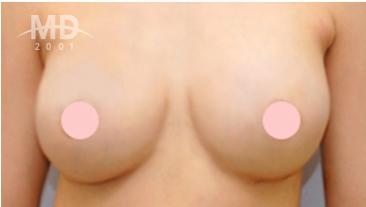
Asymmetry (difference in size)
-
Cause
- In the event of having inserted implant in wrong location or crookedly
- In the event of made erroneous measurement prior to the surgery although the breasts of the patient are congenitally asymmetric
-
Symptoms
- Breasts are not cosmetically appealing due to differing size and shape between the breasts.
-
MD's Solution
- After having removed the existing implant, correctly take measurement and insert new implant with sizes that will ensure symmetry between the breasts.
Congenital asymmetry of breasts
Asymmetric breast(difference in size) occurs more frequently due to congenital cause rather than erroneous surgical procedure. In the case of very minute asymmetry, it would not be a problem since the patients themselves are not aware of it. However, if the extent of asymmetry is severe, it can be corrected by differing the size of implant to be inserted into each of the breasts to achieve symmetry.-

Size differs
-
Height of nipple differs
-
Height of nipple and extent of sagging differ
-
Height of nipple, extent of sagging and size of areola differ
-
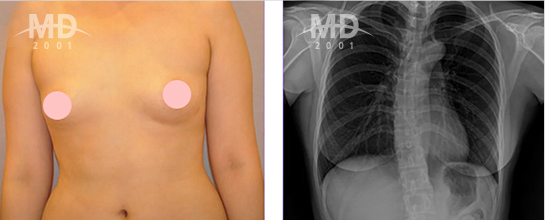
Asymmetry due to deformation of spine
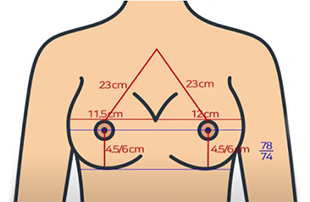
Correct asymmetry by accurately discerning
the extent of asymmetry on both sides by measuring
various sections of the breast prior to the surgery
and then differing the shape and size of each implant.
-
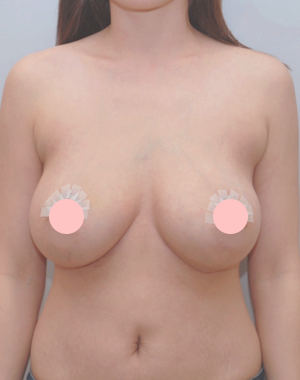
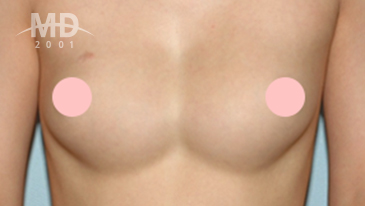
Before
-
After
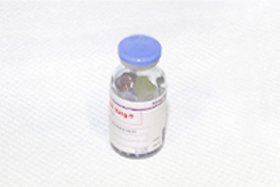
Implant rupture/replacement
-
Cause
- Case of hardened capsular due to formation of capsular contracture continuously compressing on the implant
- Case of implant ruptures on its own with passage of time, although highly rare
-
Symptoms
-
Even if implant is ruptured, gel does not leak out and pain is not induced.
Moreover, breast shape does not change significantly.
As such, it is difficult to discern whether it has ruptured based on perceived symptoms and there
-
Even if implant is ruptured, gel does not leak out and pain is not induced.
-
MD's Solution
- Remove the ruptured implant and capsular in the surrounding to create clean breast pocket before inserting new implant.
- It is possible to completely remove ruptured implant only by making incision at areola or inframammary fold .
* white arrow = ruptured implant
-
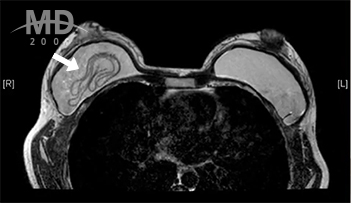 MRI scan
MRI scan
-
 Ultrasound examination
Ultrasound examination

Since there is no clear perceived symptom at the time
of implant rupture, it is essential for the patient
to undergo regular breast examination at the interval of
2 years for those in their 30’s and 1 year for those in their 40’s!
-
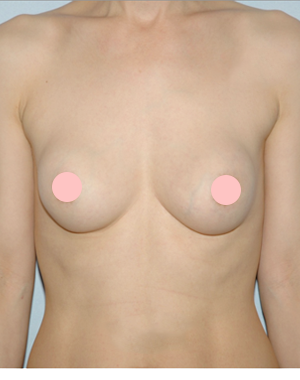
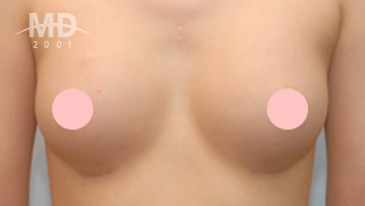
Before

-
After
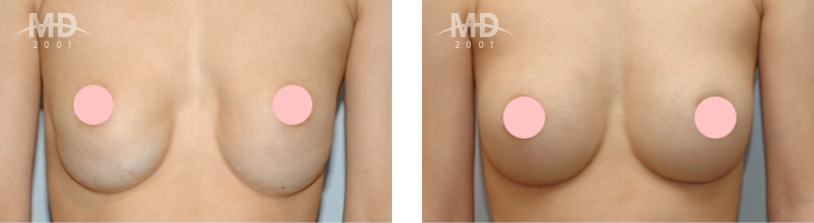
Double line

-
Cause
- If the distance between the nipple and the inframammary fold is short, exfoliation must be performed even for the areas further below the existing breast line. It can manifest if the inframammary fold has not been treated properly or if breast sags after childbirth.
-
Symptoms
- Double creases at the inframammary fold of the breast are formed due to creation of curvature in the area below the breast.
-
MD's Solution
- Remove the double creases by inserting larger implant and lift up the position of the inframammary fold .
- Depending of given situations, concurrently perform breast lifting procedure of pulling up the nipple and the sagging breast simultaneously.
-
Before

-
After
Bottoming out breast implant
-
Definition
- Phenomenon of implant being lowered or leaning to one side as an opposite phenomenon of protrusion of upper portion.
-
Cause
- When the bottom breast is small, there is insufficient support tissues, thereby causing sagging down of implant without being able to withstand its weight.
-
Symptoms
- Inframammary fold is lowered significantly unnaturally
-
MD's Solution
- Remove the capsular in the relevant area by as much as the lowering of the implant and suture the area of removal to induce lifting up of the inframammary fold , and perform additional exfoliation to secure additional space at the area above the breast.
-
Before
-
After
-
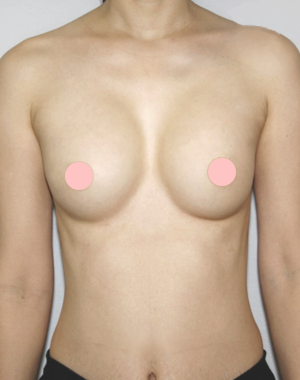
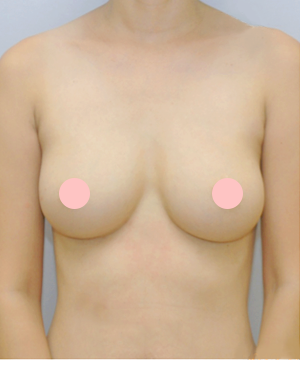
Before
-
After
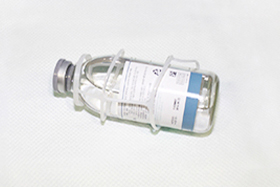
[The implant and capsular of patients who underwent thoracic implant removal from MD]
MD's procedure for removal of the breast implant
-
STEP 01.
-
STEP 02.
Discharge on the same day
(No blood bag, Can come
to work the next day) -
STEP 03.
Wearing a compression
bandage for a week
(not wearing a compression suit)
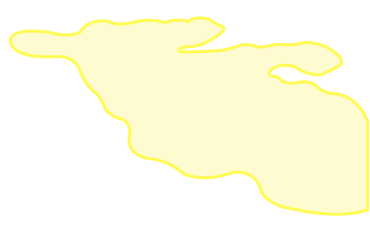
remove the capsular

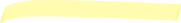
When removing (replacing) the breast implant due to side effects,
the entire capsular must be removed. However, when removing the
breast implant due to personal dissatisfaction, the capsular may
not be removed or may only be partially removed.
-
Side effects
(Capsular contracture, Implant rupture,
Seroma, calcification, etc) Complete capsulectomy
Complete capsulectomy -
Implant replacement
 Complete capsulectomy
Complete capsulectomy
or Partial capsulectomy(Determined based on ultrasound results)
-
Simple removal of implant
(Unsatisfactory shape and size)
 No capsulectomy required
No capsulectomy required(Can remove partial capsulectomy
depending on inspection result)
MD doesn't recommend complete capsulectomy unconditionally!
Even when performing breast cancer surgery at a general hospital,
only what is necessary, whether it is total resection or partial resection,
is resected. As such, MD only recommends surgery that patients need.
The same goes for capsulectomy.
The basic principle is to complete capsulectomy when reoperation is performed,
but depending on the results of ultrasound examination, the benefits and losses of
complete capsulectomy and partial capsulectomy should be considered.
Unconditionally removing 100% of the capsular
is never a good surgery and
is not a path for patient safety.
MD's judgment is simple!
-
Capsulectomy required“Complete capsulectomy (100%)”
-
No capsulectomy required“Partial capsulectomy” or “No capsulectomy”
-
No capsulectomy is required, but
100% capsulectomy is possible if the patient wants.
(If there are any risk factors for capsulectomy, consult with the patient after prior guidance)
Type of capsulectomy
| Type | Complete capsulectomy (100% capsulectomy is possible) |
Partial capsulectomy |
|---|---|---|
| Removed capsular |

|
|
| Scope of removal | 100% elimination to the bottom and back capsular that are difficult to remove |
Remove only a part of the capsular |
| The object of surgery | Recommended for side effects such as Capsular contracture, Implant rupture, Seroma, Calcification, etc |
Recommended for simple removal of implant without any side effects |
| Features | Experienced specialists need to operate as side effects such as bleeding, hematoma, and nerve damage can occur |
Based on the ultrasound results, it is necessary to determine whether there is no problem just by partial capsulectomy |
#
It is not the case that removal of capsular is advantageous unconditionally.
There are advantages in leaving the capsular intact rather than removing it!
If the implant is removed, breast gradually becomes flattened.
At this time it is possible to prevent sudden adhesion due to the presence of the capsular,
thereby playing the positive role of inducing flattening of the breast while maintaining its shape.
The capsular caused by side effects must be removed,
but there is no problem at all without removing the thin and healthy normal capsular.
-
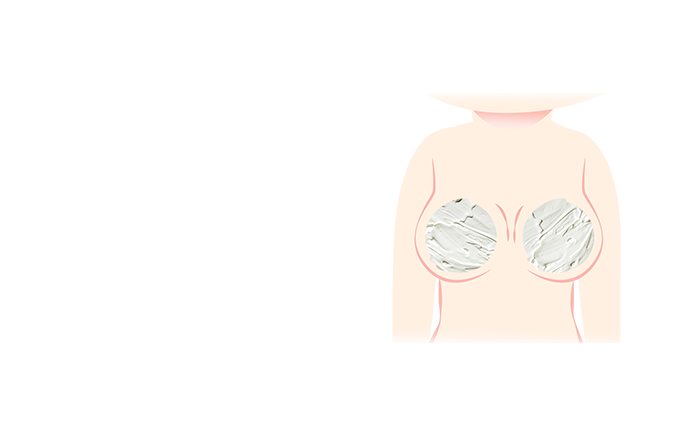
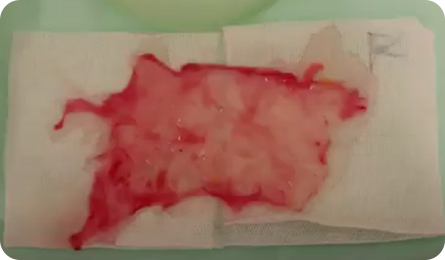
Before removing the implant
-

After removing the implant (not removing the capsular)
-

Since capsular is made of fibers in the body, it is not harmful even if it remains in the body.
-

Thin capsular will gradually contract and become naturally absorbed by the body even if it is not removed,
and will disappear by leaving slight trace. -

The assertion that capsular can induce rare cancer called anaplastic large cell lymphoma is at a very low probability.
-

On the contrary, if the capsular is removed unnecessarily,
greater side effects such as hematoma, pain, crumpling of breast, etc. can be induced.
The Ministry of Food and Drug Safety has never approved filler injections for breast expansion.
The filler is injected through a syringe into the breast without an outer shell, so you don't know where it will
spread in the body and can actually flow down to the stomach and groin.
-
A filler that drips down the breast
-
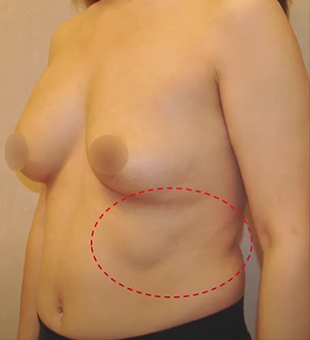
A filler that ran down to the side
-
01
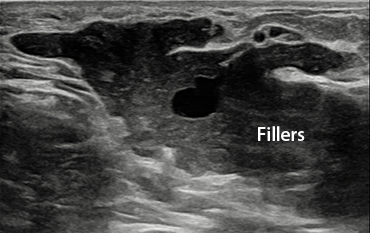
Ultrasound to locate the filler
-
02
Approximately 3-4cm areola
incision (Inframammary fold or
armpit incision is also possible
depending on where the filler is
spread in the body) -
03

Remove the lumpy fillers and the
fillers on the breast tissue
as much as possible
MD's unique surgical features to remove filler injected into the breast
Safely remove as much filler as possible without damaging the tissue!-
The maximum amount
of filler can be removed
because the filler is
removed through
incision rather than
simple suction surgery -
Know-how based on
more than 20 years of
experience enables
safe surgery without
damage to breast tissue
and blood vessels -
(Optional) Additional breast
augmentation as a safe way
to insert a implant after filler
removal surgery

Removing breast tissue as much as possible without damaging it!
-
A state in which the filler is clumped over the muscles
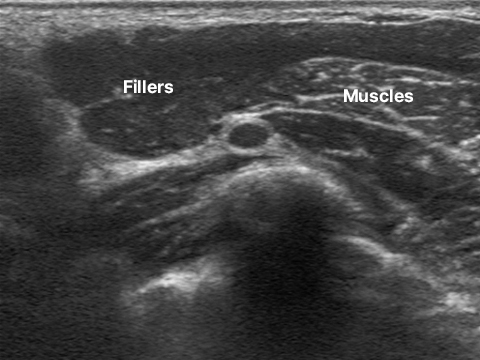
Before removal surgery
-
Fillers removed cleanly
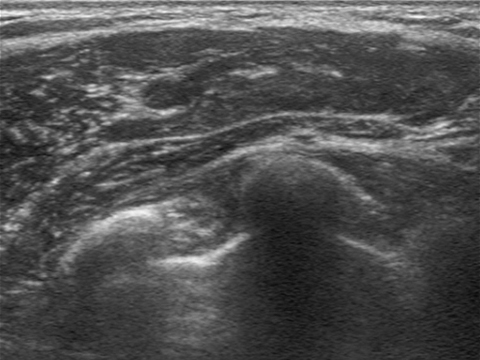
After removal surgery

-
Q1.
Fillers injected into the breast, is it absorbed?
It can't be absorbed.
However, when the filler enters the body, it is eaten by white blood cells, so the dose gradually decreases, which some doctors describe as "absorption." The general public thinks that "absorption" disappears automatically over time, but it actually remains in the body. -
Q2.
The fillers injected into the face are FDA approved, but the breast has never been approved.
Such a dangerous breast filler, why do you still do the procedure?This is because I think filler injection is simple compared to surgery to anesthetize, incision, and implant. Also, I think it's okay to put a filler in the body that is not wrapped in the outer shell in the first place, while fearing that the implant will rupture and leak out the contents. -
Q3.
Why is implant safer than filler?
The contents of the cohesive gel implant, which are currently used, are wrapped in an outer shell. The implant is less likely to rupture, but even if it ruptures, the contents do not spread into the body because it is in a highly cohesive gel state. In addition, fillers are much more dangerous because they are foreign substances not approved by the Ministry of Food and Drug Safety, not medical silicone that has been proven to be safe. -
Q4.
Is it safe to insert a implant after removing the filler injected into the breast?
Yes, no problem at all. You can remove the filler around the breast muscles where the implant will be inserted, and insert the implant. Many people come for reoperation later because their breast is small after removing the filler, and you can save money and time by removing the filler and performing implant insertion surgery at the same time.
MD proves its capabilities with results.
 Mammoplasty, why MD?
”
Mammoplasty, why MD?
”
-

Soft tactile sense that is
more real than the real thing -


Spreads out when lying down and,
when standing,
Natural waterdrop shape -


Safe surgery that reduced Bleeding
and side effects
Tactile senses
+Shape
+Safety
POINT 01
Specialized surgical technique
Is only available at MD-
Minimum
Bleeding -
Little
pain -
Quick
ecovery -
Prevention
of side
effects
-
 Intercostal nerve block to breast surgery
Intercostal nerve block to breast surgeryIntercostal nerve is a sensory nerve that conveys pain in thorax to cerebrum,
and it is possible to reduce pain by blocking it in advance before pain is
conveyed to the brain by performing intercostal nerve block prior to the surgery. -
 Bloodless breast surgery
Bloodless breast surgeryIt is possible to prevent pain and side effects that can occur due to
hemorrhage in advance by performing preventive
hemostasis in area of risk of hemorrhage.
POINT 02
Lifetime After-Sales Service Guarantee
Healthy breast is as important as beautiful breast!
-

Regular Check-Up After Surgery: One check-up after surgery
-

Visit our hospital whenever necessary for lifetime AS thereafter
POINT 03
Safe anesthetic system
We are staffed with specialist in anesthesiology capable of coping with emergency situationsand equipped with the latest general hospital level anesthetic equipment.
-
Baek Seung-hee director
Full-time presence of specialist in anesthesiology -

Anesthetics equipment
Capable of performing accurate and safe anesthesia with built-in pressure detector -

Digital monitor
Can measure vital signs of the patients including oxygen saturation level, ECG, breathing pattern, heart rate, breathing rate, blood pressure and body temperature, etc. -

Infusion pump
Injects medicine consistently into the patient at accurate pace -

Central gas pressure equipment
Real-time monitoring to prevent emergency situation of sudden drop in oxygen level
POINT 04
Convenient one-stop system
Breast examination prior to the surgery Only the examinations necessary for each individual are conducted.
-

Mammogram
-

Ultrasound
-

Chest X-Ray
-

Electrocardiogram
-

Blood test
POINT 05
Premium follow-up management
Perfect care service that does not miss out on anything including tactile senses, scars and skin recovery, etc.- Improved Tactile Sensation
- Scar Reduction
- Prevention of Capsular Contracture
- Skin regeneration
- developed by MD
-
Weekdays : AM 9:00 ~ PM 6:00
 Treatment hours
Treatment hours
Saturday : AM 9:00 ~ PM 4:00
wendsday / sunday / Closed on holidays -
3-8th floor, MD Clinic Building, 814 Seolleung-ro, Gangnam-gu, Seoul, Republic of Korea
 address
address
Privacy policy
collection: Personal information such as name, date of birth, and contact information
purpose of collection: Contact purpose for fulfillment of reservation service
retention period : 1 year (if reservation purpose is confirmed)


Find ID/Password
- Find ID
- Find Password
idHere